Pharmacogenomics Kit - Personalized Medicine DNA Test Kit


Steps of the test
-
Step 01
Order you test
-

Step 02
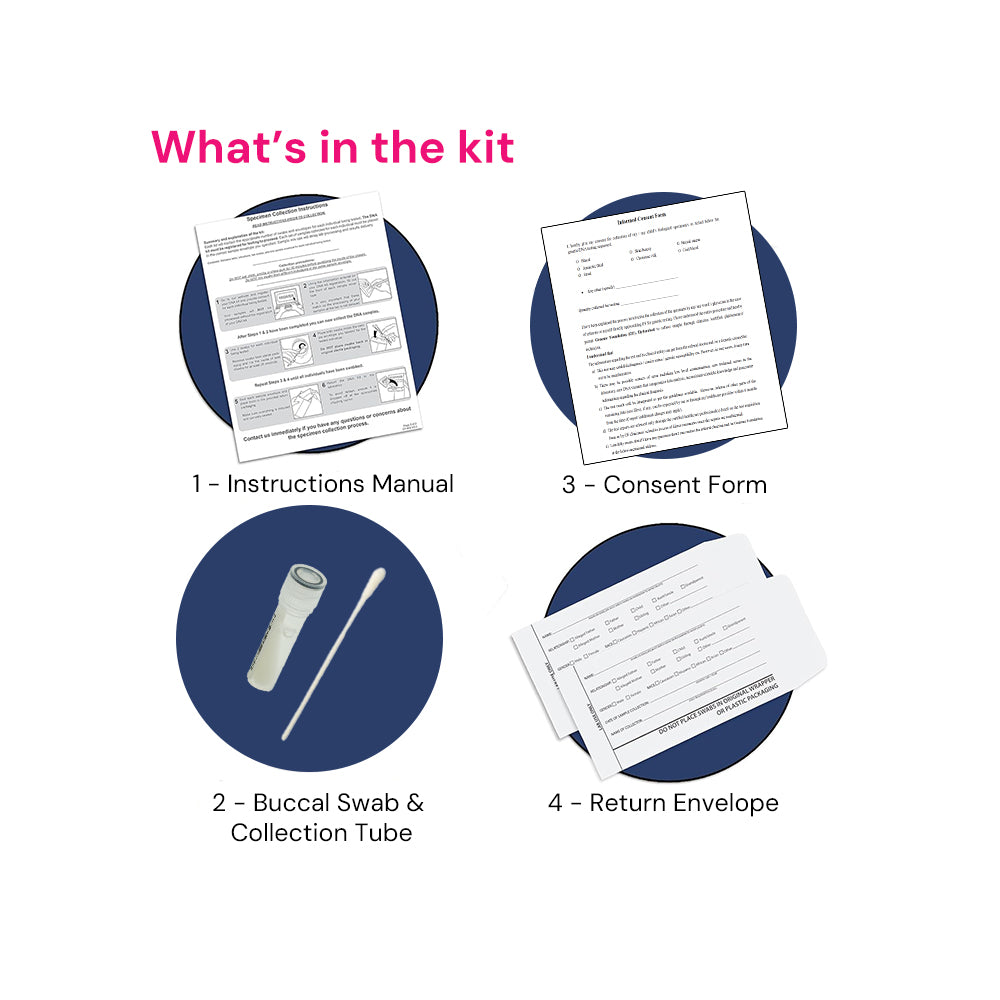
Receive the kit at your house address
-

Step 03
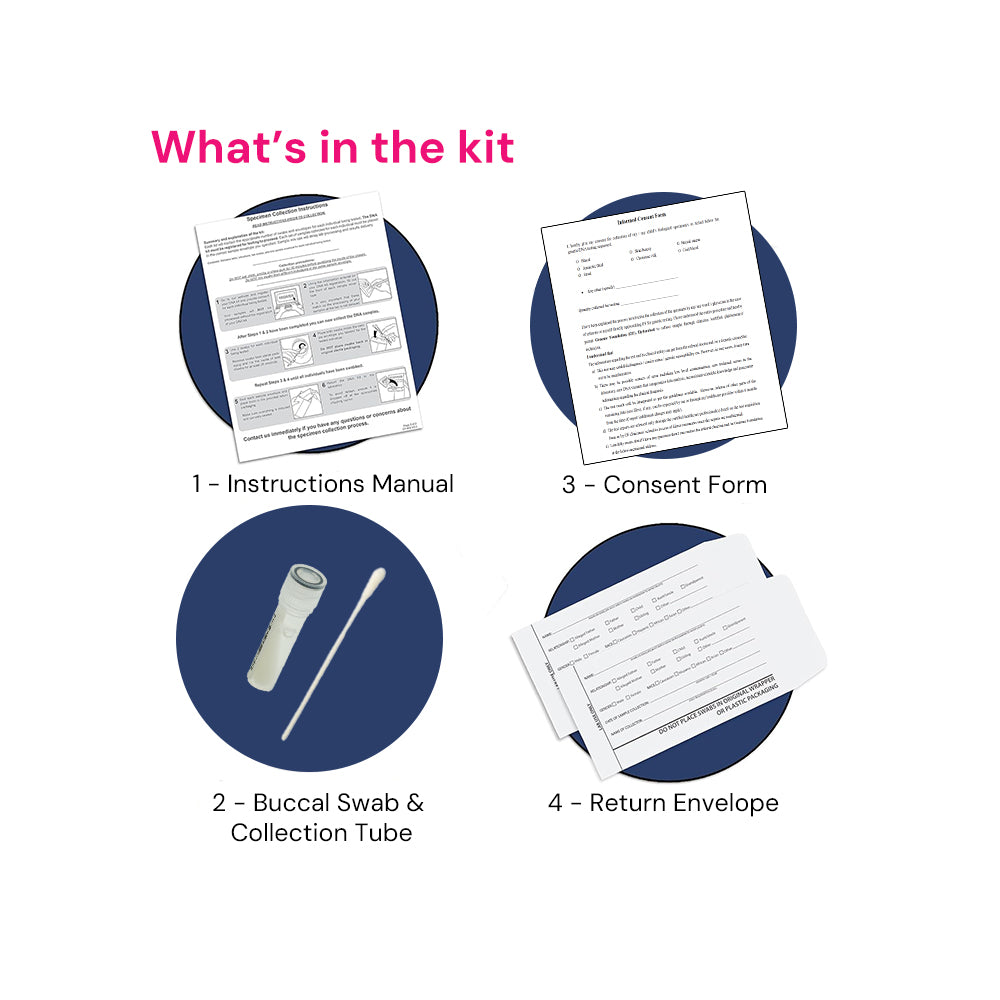
Collect your Buccal / mouth swab within 2 days of receiving the kit
-

Step 04
Connect with us so that we can schedule the reverse pick up of sample
What to Expect
About 3–4 weeks after we receive your cheek swab sample, you’ll get an email and WhatsApp notification that your personalized "Pharmacogenomics Report" is ready. Here’s what happens behind the scenes:
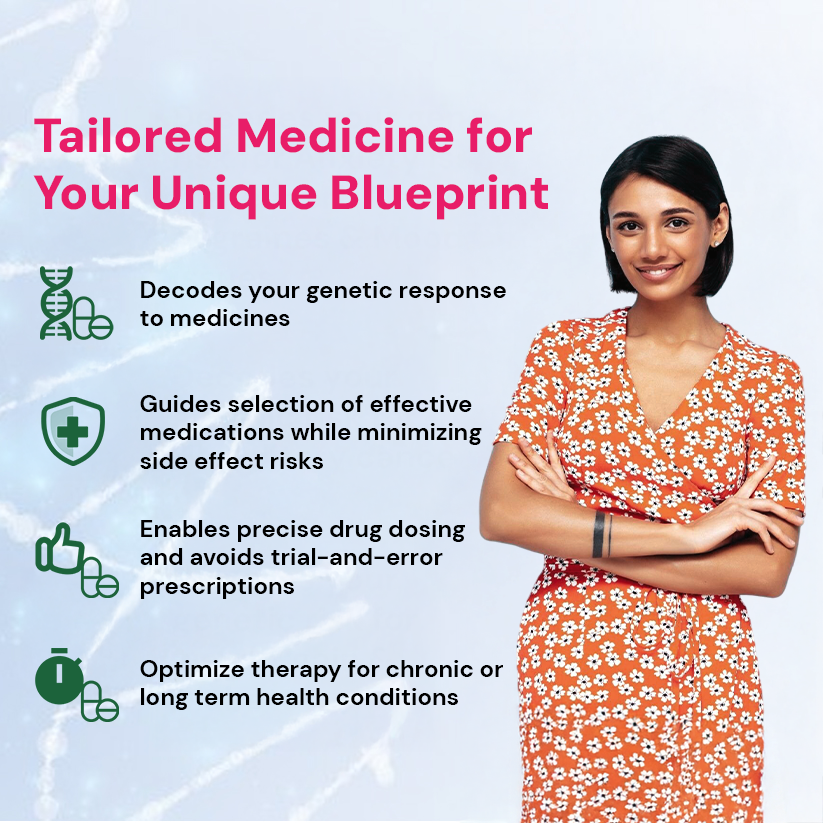
✨ This ensures you move from a “one-size-fits-all” prescription to a tailored medicine plan for a safer and effective treatment goals.
- We receive your buccal swab sample.
- Our lab team extracts DNA from your buccal sample with the highest quality standards.
- Your sample is assigned a unique ID to ensure secure and confidential processing.
- Your DNA is analyzed using advanced Next-Generation Sequencing (NGS) / high-resolution genotyping platforms.
- We scan key gene variants (such as CYP2D6, CYP2C19, SLCO1B1, TPMT, etc.) known to affect drug response.
- Rigorous quality control ensures accuracy and reliability of results.
- Our bioinformatics team matches your genetic profile with ACMG/AMP GATK, CPIC approved guidelines.
- We identify how your genes influence your response to cardiac drugs, antidepressants, painkillers, cholesterol-lowering agents, cancer therapies, and more.
- Each result is reviewed by genetic experts for clinical accuracy.
- You receive a comprehensive, easy-to-understand Pharmacogenomics Report.
- The report highlights:
- Which medicines are most effective for you
- Which medicines may cause side effects
- Recommended dose adjustments (if applicable) - Our certified genetic counselor connects with you to explain results and guide you (and your doctor) on next steps for personalized treatment decisions.
Frequently Asked Questions (FAQs)
What is pharmacogenomics testing?
Pharmacogenomics (also called pharmacogenetics) is the study of how your genes affect your response to medicines. By analyzing specific genetic variants, this test helps doctors choose the right drug, in the right dose, while reducing side effects.
How is the test performed?
The test is done using a simple buccal swab (cheek swab). No needles or blood draw are required. Your DNA is extracted from cheek cells and analyzed using Next-Generation Sequencing (NGS) or high-resolution genotyping platforms.
How is this different from a regular health check-up?
Routine check-ups measure your current health status (cholesterol, sugar, liver function, etc.). Pharmacogenomics looks at your genetic blueprint, which does not change with time, and predicts how your body will respond to medicines now and in the future.
Which medicines are covered in this test?
The test evaluates genes that influence responses to drugs in multiple therapeutic areas:
- Cardiovascular – Blood thinners (warfarin, clopidogrel), anticoagulants (apixaban, dabigatran, rivaroxaban), anti-arrhythmics (flecainide, propafenone), antihypertensives (beta-blockers, ACE inhibitors, ARBs, diuretics, calcium-channel blockers), and statins (atorvastatin, rosuvastatin, simvastatin, pravastatin, lovastatin).
- Psychiatric – Antidepressants (sertraline, fluoxetine, venlafaxine, paroxetine, amitriptyline, escitalopram, citalopram, duloxetine, etc.) and antipsychotics (risperidone, olanzapine, clozapine, quetiapine, aripiprazole, lithium).
- Pain management – Analgesics/NSAIDs (acetaminophen, naproxen, sulindac) and opioids (tramadol, oxycodone, methadone, fentanyl, tapentadol, buprenorphine).
- Diabetes – Metformin, sulfonylureas (glimepiride, gliclazide, glibenclamide, glipizide), DPP-4 inhibitors (sitagliptin, vildagliptin, linagliptin), SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin), GLP-1 agonists (liraglutide, semaglutide), and thiazolidinediones (pioglitazone, rosiglitazone).
- Oncology (cancer therapy) – Chemotherapy agents such as mercaptopurine (TPMT variants), irinotecan (UGT1A1 variants), and targeted therapies like trastuzumab (HER2 status), with side-effect and toxicity risk prediction.
- Immunology & Transplant – Immunosuppressants including azathioprine, tacrolimus, cyclosporine, mycophenolate, and biologics (adalimumab, infliximab, etanercept) used in autoimmune conditions and post-transplant care.
- Other conditions – Gastrointestinal (PPIs such as omeprazole, esomeprazole, lansoprazole, pantoprazole), antiemetics (granisetron, palonosetron), asthma (tiotropium, glucocorticoids), and anti-inflammatory/arthritis drugs (methotrexate, allopurinol, TNF-inhibitors).
How accurate is the test?
Our test follows internationally recognized guidelines (ACMG/AMP GATK, CPIC). The sequencing is performed at >95% coverage and high depth to ensure robust and clinically relevant results. However, genetic testing is one piece of information and should always be interpreted along with your medical history and doctor’s advice.
Is pharmacogenomic testing useful for everyone?
Yes. Even healthy individuals can benefit by knowing how their body may react to common medicines in the future. For patients already on multiple medications, it helps avoid trial-and-error prescribing and prevents adverse drug reactions.





 100% Quality Guarantee
100% Quality Guarantee Free Delivery
Free Delivery Expert consultation with Pharmacogenomist
Expert consultation with Pharmacogenomist